Do I Suffer Overpronation Of The Feet
Normal, healthy feet pronate! Normal pronation does not need to be ?corrected?. However, some people OVER-pronate. Those people need a shoe that supports their over-pronating foot to help guide the foot and avoid injury. So, what does pronation mean exactly? Well, ?pronate? is the word used to describe the natural motion of the foot after it strikes the ground. When a person with a normally pronating foot runs, the outside part of the heel strikes the ground. As the individual shifts the body weight forward, the foot rolls inward (pronates) and the entire foot comes into contact with the ground. This allows the foot to properly support the body and absorb the impact forces. Motion continues forward and the peron pushes off (called ?toe off?) evenly from the front of the foot. Someone who OVER-pronates strikes the ground with the heel in the same way, but the foot rolls too far inward (overpronation). This causes foot and ankle strain, as it does not allow the foot and ankle to properly support the body nor to properly absorb the impact forces. As motion continues forward, they will toe-off more from the ball of her foot. Runners who overpronate are susceptible to foot, ankle and knee problems if they don't wear a shoe that properly supports the motion of their feet.

Causes
You do not have to be a runner or athlete to suffer from overpronation. Flat feet can be inherited, and many people suffer from pain on a day-to-day basis. Flat feet can also be traumatic in nature and result from tendon damage over time. Wearing shoes that do not offer enough arch support can also contribute to overpronation.
Symptoms
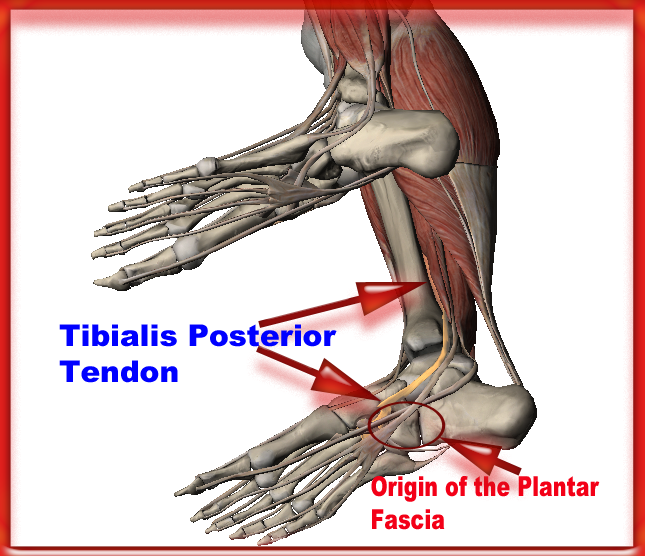
People with overpronation may suffer from pain in the knees, hips, and low back. Overpronation itself does not necessarily cause any other symptoms but is a contributing factor of many foot conditions such as Plantar Facsiitis, Heel Spur Syndrome, Posterior Tibialis Tendon Rupture or Tendonitis, Hallux Valgus, Bunion Deformities, Metatarsalgia, Hallux Limitus or Hallux Rigidus, Hammer Toes, and Morton?s Neuroma.
Diagnosis
When you overpronate your foot rolls inwards causing the lower leg to rotate inwards too. It's thought that this increases stress on the soft tissues of the lower leg causing pain and inflammation, or more commonly known as shin splints.

Non Surgical Treatment
Flat feet and fallen arches can be treated effectively by wearing an orthotic insert in your shoes. Orthotics can be custom-made and prescribed by your foot specialist (podiatrist), or you can use a so called pre-made foot orthotic. Most people do not require expensive custom-made orthotics to combat excess pronation, unless they have a specific medical foot condition. Footlogics orthotic insoles were developed to correct excess pronation, thereby providing sustainable, long-lasting pain relief to many aches and pains in a natural way. Footlogics Comfort, Casual and Sports are products which promote excellent biomechanical control of the foot.
Surgical Treatment
HyProCure implant. A stent is placed into a naturally occurring space between the ankle bone and the heel bone/midfoot bone. The stent realigns the surfaces of the bones, allowing normal joint function. Generally tolerated in both pediatric and adult patients, with or without adjunct soft tissue procedures. Reported removal rates, published in scientific journals vary from 1%-6%.
Should I Address Calcaneal Apophysitis From Home?
Sever's disease is a term used to describe inflammation of the calcaneal apophysis which occurs in children and adolescents. Sever first described the condition in 1912. Further studies have suggested that the condition is due to repeated 'microtrauma' at the site of the attachment of the Achilles tendon to the apophysis of the heel, often as result of sporting activities. The disorder can be classified among the general osteochondrosis syndromes such as Osgood-Schlatter disease.
Causes
Sever?s disease is caused by repetitive tension and/or pressure on the growth center of the heel. Running and jumping place a large amount of pressure on the heels and can cause pain. Children with Sever?s may limp or have an altered gait due to the pain. Risk factors for Sever's include tight calf muscles, weak ankle muscles, and alignment abnormalities at the foot and ankle. Sever?s can also result from wearing shoes without sufficient heel padding or arch support.
Symptoms
Signs and symptoms of Sever?s disease include heel pain can be in one or both heels, and it can come and go over time. Many children walk or run with a limp, they may walk on their toes to avoid pressure on their heels. Heel pain may increase with running or jumping, wearing stiff, hard shoes (ex. soccer cleats, flip-flops) or walking barefoot. The pain may begin after increasing physical activity, such as trying a new sport or starting a new sports season.
Diagnosis
Sever disease is most often diagnosed clinically, and radiographic evaluation is believed to be unnecessary by many physicians, but if a diagnosis of calcaneal apophysitis is made without obtaining radiographs, a lesion requiring more aggressive treatment could be missed. Foot radiographs are usually normal and the radiologic identification of calcaneal apophysitis without the absence of clinical information was not reliable.
Non Surgical Treatment
Sever?s disease will go away on its own with rest or after heel bone growth is complete, usually within 2 to 8 weeks after the heel pain or discomfort appears. Sever?s disease is not expected to cause long-term problems, though symptoms may linger for up to several years in severe cases. Certain conservative care measures may be helpful in treating this health problem, including avoiding activities that provoke pain or discomfort, elevating the leg while at rest, performing hamstring and calf muscle stretches two to three times per day, undergoing physical therapy, using cold therapy, using an elastic wrap or compression stocking, Avoiding footwear with heel elevation, toe spring, and toe taper, and instead favoring footwear that?s completely flat and widest at the ends of the toes. More aggressive treatment measures, including over-the-counter anti-inflammatory medication (e.g. ibuprofen), steroid injections, and surgery, may be indicated in certain cases. Addressing the footwear component of this health problem is an important part of a well-rounded Sever?s disease treatment plan. Optimal footwear for preventing or treating this problem is flat, wide (widest at the ends of the toes), and flexible in the sole. Open-back footwear (such as certain Crocs models) may be particularly helpful for kids and teens with Sever?s disease.
Prevention
Sever's disease may be prevented by maintaining good joint and muscle flexibility in the years leading up to, and during, their growth spurts (eg girls 8 to 10, boys 10 to 12). Foot arch problems such as flat feet should be addressed after the age of five if they don't appear to be self-correcting. If you are concerned, please ask your health practitioner. The most important factor is the amount of weight-bearing exercise your child is currently performing. Finally, LISTEN To Your Child! If your child is suffering heel pain between the ages of 8 to 12, suspect Sever's disease until proven otherwise. Seek the professional opinion of your foot practitioner regarding its diagnosis and subsequent management.
Acquired Flat Foot Tibialis Posterior Pain
Overview
Some people have always had flat feet from a young age. Unfortunately as people reach their fifties they will suddenly have one foot with a flatter arch than the other foot. This situation is termed adult acquired flatfoot. Adult acquired flatfoot is a painful condition occurring in one foot. The common patient profile is a female over the age of 50 with pre-existing flatfeet, high blood pressure, high cholesterol, diabetes and obesity. All of these underlying problems will lead to a weakening of the support structures of the arch. If you have adult acquired flat foot you will not be able to lift your heel off the ground while standing on one leg. Adult acquired flatfoot may develop due to trauma or degeneration of major tendons ankle & foot. Weakness or paralysis of leg muscles can also create a flatfoot deformity. 
Causes
The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur.
Symptoms
Often, this condition is only present in one foot, but it can affect both. Adult acquired flatfoot symptoms vary, but can swelling of the foot's inner side and aching heel and arch pain. Some patients experience no pain, but others may experience severe pain. Symptoms may increase during long periods of standing, resulting in fatigue. Symptoms may change over time as the condition worsens. The pain may move to the foot's outer side, and some patients may develop arthritis in the ankle and foot.
Diagnosis
Examination by your foot and ankle specialist can confirm the diagnosis for most patients. An ultrasound exam performed in the office setting can evaluate the status of the posterior tibial tendon, the tendon which is primarily responsible for supporting the arch structure of the foot.
Non surgical Treatment
Depending on the stage of the deformity and patient?s functional goals, various treatment options are available. Some patients improve with conservative care which includes rest and immobilization, shoe modifications, orthoses and bracing, or physical therapy. Surgery might be warranted for advanced stages of the condition. Often a combination of procedures including tendon and muscle augmentation, tendon transfers, realigning of bones or fusion of certain joints might be necessary in more advanced cases. Your doctor will evaluate and recommend an individualized plan of care with your specific needs in mind. 
Surgical Treatment
Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss.
Adult Aquired Flat Foot Do I Suffer From AAF?
Most flat feet are not painful, particularly those flat feet seen in children. In the adult acquired flatfoot, pain occurs because soft tissues (tendons and ligaments) have been torn. The deformity progresses or worsens because once the vital ligaments and posterior tibial tendon are lost, nothing can take their place to hold up the arch of the foot. The painful, progressive adult acquired flatfoot affects women four times as frequently as men. It occurs in middle to older age people with a mean age of 60 years. Most people who develop the condition already have flat feet. A change occurs in one foot where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Why this event occurs in some people (female more than male) and only in one foot remains poorly understood. Contributing factors increasing the risk of adult acquired flatfoot are diabetes, hypertension, and obesity.

Causes
A person with flat feet has greater load placed on the posterior tibial tendon which is the main tendon unit supporting up the arch of the foot. Throughout life, aging leads to decreased strength of muscles, tendons and ligaments. The blood supply diminishes to tendons with aging as arteries narrow. Heavier, obese patients have more weight on the arch and have greater narrowing of arteries due to atherosclerosis. In some people, the posterior tibial tendon finally gives out or tears. This is not a sudden event in most cases. Rather, it is a slow, gradual stretching followed by inflammation and degeneration of the tendon. Once the posterior tibial tendon stretches, the ligaments of the arch stretch and tear. The bones of the arch then move out of position with body weight pressing down from above. The foot rotates inward at the ankle in a movement called pronation. The arch appears collapsed, and the heel bone is tilted to the inside. The deformity can progress until the foot literally dislocates outward from under the ankle joint.
Symptoms
Pain and swelling behind the inside of your ankle and along your instep. You may be tender behind the inner ankle where the posterior tibial tendon courses and occasionally get burning, shooting, tingling or stabbing pain as a result of inflammation of the nerve inside the tarsal tunnel. Difficulty walking, the inability to walk long distances and a generalised ache while walking even short distances. This may probably become more pronounced at the end of each day. Change in foot shape, sometimes your tendon stretches out, this is due to weakening of the tendon and ligaments. When this occurs, the arch in your foot flattens and a flatfoot deformity occurs, presenting a change in foot shape. Inability to tip-toe, a way of diagnosing Posterior Tibial Tendon Dysfunction is difficulty or inability to ?heel rise? (stand on your toes on one foot). Your tibialis posterior tendon enables you to perform this manoeuvre effectively. You may also experience pain upon attempting to perform a heel rise.
Diagnosis
The history and physical examination are probably the most important tools the physician uses to diagnose this problem. The wear pattern on your shoes can offer some helpful clues. Muscle testing helps identify any areas of weakness or muscle impairment. This should be done in both the weight bearing and nonweight bearing positions. A very effective test is the single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward). X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the imaging modality of choice for evaluating the posterior tibial tendon and spring ligament complex.
Non surgical Treatment
Treatment of Adult Acquired Flatfoot Deformity depends on the stage of progression, as mentioned above paragraphs. Below we will outline a variety of different treatment options available. Orthotics or bracing. To give your foot the arch the support it needs, your podiatrist or foot specialist may provide you with over the counter brace or a custom orthotic device that fits your shoe. Casting. In some cases, a cast or boot is worn to stabilize the foot and to give the tendon time to heal. Physiotherapy. Ultrasound treatments and exercises may help rehab the tendon and muscles. Medications. Over-the-counter (NSAIDS) such as ibuprofen can help reduce pain, inflammation and swelling associated with AAFD. Shoe Gear. Your podiatrist may suggest changes with your shoes you are wearing and inserts you need in your shoe to help support your arch.

Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Symptomatic flexible flatfoot conditions are common entities in both the adolescent and adult populations. Ligamentous laxity and equinus play a significant role in most adolescent deformities. Posterior tibial tendon dysfunction (PTTD) is the most common cause of adult acquired flatfoot. One should consider surgical treatment for patients who have failed nonoperative therapy and have advancing symptoms and deformities that significantly interfere with the functional demands of daily life. Isolated Joint Fusion. This technique is used for well reducible flat foot by limiting motion at one or two joints that are usually arthritic. The Evans Anterior Calcaneal Osteotomy. This is indicated for late stage II adult acquired flatfoot and the flexible adolescent flatfoot. This procedure will address midtarsal instability, restore the medial longitudinal arch and reduce mild hind foot valgus. The Posterior Calcaneal Displacement Osteotomy (PCDO). This technique is indicated for late stage I and early stage II PTTD with reducible Calcaneal valgus. This is often combined with a tendon transfer. A PCDO is also indicated as an adjunctive procedure in the surgical reconstruction of the severe flexible adolescent flatfoot. Soft tissue procedure. On their own these are not very effective but in conjunction with an osseous procedure, soft tissue procedures can produce good outcome. Common ones are tendon and capsular repair, tendon lengthening and transfer procedures. Flat foot correction requires lengthy post operative period and a lot of patience. Your foot may need surgery but you might simply not have the time or endurance to go through the rehab phase of this type of surgery. We will discuss these and type of procedures necessary for your surgery in length before we go further with any type of intervention.
What Could Cause Achilles Tendinitis ?
 The Achilles tendon connects the calf muscle to the back of the heel. Injuries to the Achilles tendon are common, as it is in constant use during walking and running. These injuries, known as Achilles tendinitis, are usually the result of overuse damage and minor tears that have accumulated over years. Your risk of developing Achilles tendinitis increases with age and activity level. Many athletes develop Achilles tendinitis. The tendon may be injured several inches away from where it attaches to the foot or at the point of attachment. An injury at the point of attachment is called Achilles enthesopathy. We recommend a combination of treatments over a period of months that may include wearing supportive shoes or orthotic devices, performing stretching exercises, and icing the affected area. If these treatments are not effective, or if the tendon is completely torn, we may recommend surgery.
The Achilles tendon connects the calf muscle to the back of the heel. Injuries to the Achilles tendon are common, as it is in constant use during walking and running. These injuries, known as Achilles tendinitis, are usually the result of overuse damage and minor tears that have accumulated over years. Your risk of developing Achilles tendinitis increases with age and activity level. Many athletes develop Achilles tendinitis. The tendon may be injured several inches away from where it attaches to the foot or at the point of attachment. An injury at the point of attachment is called Achilles enthesopathy. We recommend a combination of treatments over a period of months that may include wearing supportive shoes or orthotic devices, performing stretching exercises, and icing the affected area. If these treatments are not effective, or if the tendon is completely torn, we may recommend surgery.
Causes
Achilles tendinitis is usually caused by straining the Achilles tendon through intense activity or a sudden increase in exercise. Individuals who play basketball often develop Achilles tendinitis as a result of pivoting, jumping, and running. These repetitive movements put pressure on the tendon and can gradually wear it down over time. Increasing the intensity of your workouts may also lead to the development of Achilles tendinitis. This is commonly seen in long distance runners who do quite a bit of uphill running. Similarly, if you start exercising more frequently you may also develop the condition due to overuse of the tendon. Not stretching properly before exercise can also make the tendon more prone to injury. Achilles tendinitis is also common in individuals whose feet have a flattened arch, as this places more stress on the tendon. The condition can also be triggered by arthritis, as joint pain can cause one to compensate by putting more pressure on the Achilles tendon.
Symptoms
Morning pain is a hallmark symptom because the achilles tendon must tolerate full range of movement including stretch immediately on rising in the morning. Symptoms are typically localized to the tendon and immediate surrounding area. Swelling and pain at the attachment are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes. With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis.
Diagnosis
To confirm the diagnosis and consider what might be causing the problem, it?s important to see your doctor or a physiotherapist. Methods used to make a diagnosis may include, medical history, including your exercise habits and footwear, physical examination, especially examining for thickness and tenderness of the Achilles tendon, tests that may include an x-ray of the foot, ultrasound and occasionally blood tests (to test for an inflammatory condition), and an MRI scan of the tendon.
Nonsurgical Treatment
Initial treatment consists of medication and ice to relieve the pain, stretching and strengthening exercises, and modification of the activity that initially caused the problem. These all can be carried out at home, although referral to a physical therapist or athletic trainer for further evaluation and treatment may be helpful. Occasionally a walking boot or cast may be recommended to immobilize the tendon, allowing the inflammation to settle down. For less severe cases or after immobilization, a heel lift may be prescribed to reduce stress to the tendon. This may be followed by an elastic bandage wrap of the ankle and Achilles tendon. Orthotics (arch supports) may be prescribed or recommended by your physician. Surgery to remove the inflamed tendon lining or degenerated tendon tissue is rarely necessary and has shown less than predictable results.

Surgical Treatment
Many people don't realize that Achilles tendon surgery can be very traumatic to your body. The type of trauma you experience after surgery can be compared to what you go through when you first injured your Achilles tendon. During the first 24 to 72 hours after the surgery your ankle will be tender, swollen and very painful. Your leg will be weak and unstable making it impossible for you to put weight on your leg without some kind of help. This is why your doctor or surgeon will have you outfitted for a cast, ankle brace and/or crutches before the procedure. When you are relying on a cast/brace and crutches your Achilles tendon is less likely to be as active as it once was. This is usually why atrophy (loss) of your lower leg muscles (specifically your calf muscle) happens. In general, more than 80%* of people who undergo surgery for an injured Achilles Tendon are able to return to their active lifestyle. In order to avoid re-injury, it is important to commit to a regular conservative therapy routine.
Prevention
Suggestions to reduce your risk of Achilles tendonitis include, incorporate stretching into your warm-up and cool-down routines, maintain an adequate level of fitness for your sport, avoid dramatic increases in sports training, if you experience pain in your Achilles tendon, rest the area. Trying to ?work through? the pain will only make your injury worse, wear good quality supportive shoes appropriate to your sport. If there is foot deformity or flattening, obtain orthoses, avoid wearing high heels on a regular basis. Maintaining your foot in a ?tiptoe? position shortens your calf muscles and reduces the flexibility of your Achilles tendon. An inflexible Achilles tendon is more susceptible to injury, maintain a normal healthy weight.
What Will Cause Heel Discomfort And Approaches To Prevent It
Overview
Plantar fasciitis is the most common cause of heel pain in runners, eventually affecting 10 percent of the running community. While running, the plantar fascia works with the Achilles tendon to store and return energy. Because of its powerful attachment to the base of the toe, the plantar fascia stabilizes the inner forefoot as forces peak during pushoff. Unlike bone spurs and stress fractures of the heel, plantar fasciitis tends to produce pain during the pushoff phase while running, not during initial contact. A simple way to tell if you have plantar fasciitis versus a heel spur/stress fracture is to walk on your toes: heel spurs and heel stress fractures feel better while you walk on your toes, while plantar fasciitis typically produces more discomfort when you shift your weight onto your toes.
Causes
Plantar fasciitis occurs because of irritation to the thick ligamentous connective tissue that runs from the heel bone to the ball of the foot. This strong and tight tissue contributes to maintaining the arch of the foot. It is also one of the major transmitters of weight across the foot as you walk or run. Therefore, the stress placed on the this tissue is tremendous.
Symptoms
Plantar fasciitis is characterized by the following signs and symptoms. Acute plantar fasciitis, pain is usually worse in the morning but may improve when activity continues; if the plantar fasciitis is severe, activity will exacerbate the pain, pain will worsen during the day and may radiate to calf or forefoot, pain may be described anywhere from "minor pulling" sensation, to "burning", or to "knife-like", the plantar fascia may be taut or thickened, passive stretching of the plantar fascia or the patient standing on their toes may exacerbate symptoms, acute tenderness deep in the heel-pad along the insertion of the plantar aponeurosis at the medial calcaneal tuberosity and along the length of the plantar fascia, may have localized swelling. Chronic plantar fasciitis, plantar fasciitis is classified as "chronic" if it has not resolved after six months, pain occurs more distally along the aponeurosis and spreads into the Achilles tendon.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
Your doctor will determine what treatment is best for your condition. The most common treatments for plantar fasciitis include icing the affected area, inserting custom-made orthotics into your shoes, massaging the plantar fascia, nonsteroidal anti-inflammatory drugs (NSAIDs), steroid injections, strengthening the foot, wearing a night splint, wearing shoes with arch support, physical therapy, stretching the calf muscles, shockwave therapy or radiotherapy. To keep the plantar fascia lengthened as you sleep, your doctor may ask you to wear night splints. In the morning, taking your first steps is less painful because the plantar fascia remains stretched throughout the night. Avoiding activities such as walking or running helps the healing process. Losing weight, if it is a factor in the condition, may help to reduce the stress placed on the plantar fascia.
Surgical Treatment
Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted. The most common complications of release surgery include incomplete relief of pain and nerve damage.
What Is Heel Discomfort And The Best Ways To Get Rid Of It

Overview
The Plantar Fascia is a strong ligament-like structure under the arch of the foot that runs from the heel bone to the ball of the foot. If we could see it in isolation it has a triangular shape when looked at from underneath but has a curved shape when looked at from the side - much like a sail boat’s sail billowing in the wind. The most functional piece is from the front-bottom-inside area of the heel bone (calcaneous) to the joint of the big toe (hallux) and this is where the majority of stress of walking (and running and jumping) is taken by the fascia. How your plantar fascia reacts to and recovers from this stress is what determines the extent and nature of your plantar fasciitis.
Causes
When some people stand/walk/run/jump their own anatomy in their ankle joint is not ‘sturdy’ enough to cope with the needed stabilisation of their ankle joint when they are weight bearing. So, their ankle rotates to find a point of stability. By the shin twisting in and the ankle rotating downwards to the inside (along with your body weight, the power of some muscles, and of course, gravity) a huge amount of stress is applied to the plantar fascia until it is stressed beyond it’s normal limits and it starts to ‘tighten up’. It is this tightening up of the plantar fascia under this stress that causes the damage that in turn leads to pain…eventually.
Symptoms
When plantar fasciitis occurs, the pain is typically sharp and usually unilateral (70% of cases).Heel pain worsens by bearing weight on the heel after long periods of rest. Individuals with plantar fasciitis often report their symptoms are most intense during their first steps after getting out of bed or after prolonged periods of sitting. Improvement of symptoms is usually seen with continued walking. Numbness, tingling, swelling, or radiating pain are rare but reported symptoms. If the plantar fascia continues to be overused in the setting of plantar fasciitis, the plantar fascia can rupture. Typical signs and symptoms of plantar fascia rupture include a clicking or snapping sound, significant local swelling, and acute pain in the sole of the foot.
Diagnosis
X-rays are a commonly used diagnostic imaging technique to rule out the possibility of a bone spur as a cause of your heel pain. A bone spur, if it is present in this location, is probably not the cause of your pain, but it is evidence that your plantar fascia has been exerting excessive force on your heel bone. X-ray images can also help determine if you have arthritis or whether other, more rare problems, stress fractures, bone tumors-are contributing to your heel pain.
Non Surgical Treatment
Your GP or podiatrist may advise you to change your footwear. You should avoid wearing flat-soled shoes, because they will not provide your heel with support and could make your heel pain worse. Ideally, you should wear shoes that cushion your heels and provide a good level of support to the arches of your feet. For women wearing high heels, and for men wearing heeled boots or brogues, can provide short- to medium-term pain relief, as they help reduce pressure on the heels. However, these types of shoes may not be suitable in the long term, because they can lead to further episodes of heel pain. Your GP or podiatrist can advise on footwear. Orthoses are insoles that fit inside your shoe to support your foot and help your heel recover. You can buy orthoses off-the-shelf from sports shops and larger pharmacies. Alternatively, your podiatrist should be able to recommend a supplier. If your pain does not respond to treatment and keeps recurring, or if you have an abnormal foot shape or structure, custom-made orthoses are available. These are specifically made to fit the shape of your feet. However, there is currently no evidence to suggest that custom-made orthoses are more effective than those bought off-the-shelf. An alternative to using orthoses is to have your heel strapped with sports strapping (zinc oxide) tape, which helps relieve pressure on your heel. Your GP or podiatrist can teach you how to apply the tape yourself. In some cases, night splints can also be useful. Most people sleep with their toes pointing down, which means tissue inside the heel is squeezed together. Night splints, which look like boots, are designed to keep your toes and feet pointing up while you are asleep. This will stretch both your Achilles tendon and your plantar fascia, which should help speed up your recovery time. Night splints are usually only available from specialist shops and online retailers. Again, your podiatrist should be able to recommend a supplier. If treatment hasn't helped relieve your painful symptoms, your GP may recommend corticosteroid injections. Corticosteroids are a type of medication that have a powerful anti-inflammatory effect. They have to be used sparingly because overuse can cause serious side effects, such as weight gain and high blood pressure (hypertension). As a result, it is usually recommended that no more than three corticosteroid injections are given within a year in any part of the body. Before having a corticosteroid injection, a local anaesthetic may be used to numb your foot so you don't feel any pain.

Surgical Treatment
Surgery should be reserved for patients who have made every effort to fully participate in conservative treatments, but continue to have pain from plantar fasciitis. Patients should fit the following criteria. Symptoms for at least 9 months of treatment. Participation in daily treatments (exercises, stretches, etc.). If you fit these criteria, then surgery may be an option in the treatment of your plantar fasciitis. Unfortunately, surgery for treatment of plantar fasciitis is not as predictable as a surgeon might like. For example, surgeons can reliably predict that patients with severe knee arthritis will do well after knee replacement surgery about 95% of the time. Those are very good results. Unfortunately, the same is not true of patients with plantar fasciitis.